In this article, Lisa Drake, Redmoor Health’s Director of Quality Improvement, shares her expertise and learnings on securing successful digital transformations in the NHS through effective procurement strategies.
I often wish I had a crystal ball…I don’t, but as someone else said recently, “As we move into the latter part of our careers, a certain ‘wisdom’ comes with it” (that’s much kinder than just being older than everyone else). Who’d have thought when I penned this blog about Finances, procurement, reorganisations, research, and new models of care a few weeks ago this would happen:
NHSE forced to suspend £300m Digital framework after a claim against it.
So, now I’m pondering a bit more about specification, procurement, engagement and implementation in the NHS. It’s a hard task to achieve this across 42 ICSs, in 7 Regions, with a market approach to innovation and choice.
There are 42 different Digital Strategies; lots of them have common themes, some of them are a bit ‘motherhood and apple pie’, with little substance on the ‘how’ they will be delivered. I wonder if any are being reconsidered now to account for this delay. We have (or thought we had) a robust procurement process, but this isn’t the first time a procurement has been suspended due to a challenge. Whilst this is the domain of experts, and I don’t profess to be anywhere in that space, we do see the impact when it goes awry.
NHS Digital Commissioning And Procurement: Specification Stage, Benefits For Who?
When we create specifications and focus primarily on the recipient of the service, i.e. the patient, we often fail to consider the middle user, the provider of the service in general practice. We also fail to consider the engagement required to help people understand the ‘why’, and the what’s in it for me. This isn’t always the same as ‘what’s in it for others. Commissioning tends to think, product first, sometimes there’s a consideration for training, but that’s after the choice has been made.
NHS Digital Commissioning And Procurement: Engagement Stage, Getting Stakeholder Buy-In
The engagement stage is crucial if you want to ensure adoption and spread, as people need not only to know what’s in it for me, but they also need to understand how much change is required to move to a new supplier and product. Because if it is only marginally better, people won’t change, they will stick with their existing product, even though they know it isn’t great.
NHS Digital Commissioning And Procurement: Case Study, Online Consultation And Video Consultation
Some of the online, video, and messaging solution specification requirements are now resulting in a lot of overlap, as each supplier is asked to offer features and functionality that perhaps are already available in another product that is well established in the marketplace.
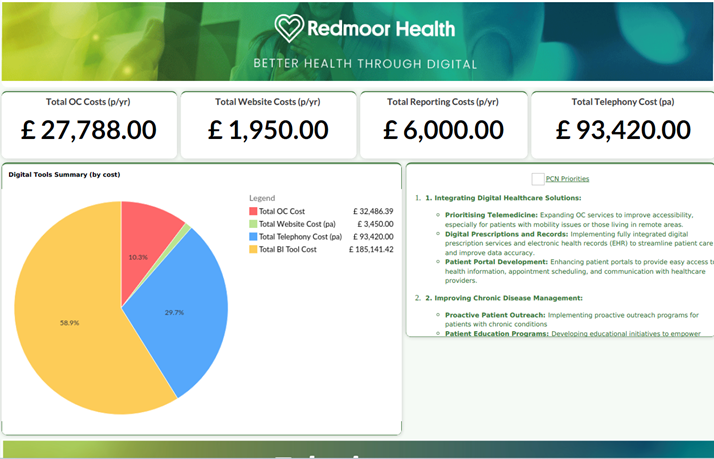
I say each time we help an ICB, please consider all your digital solutions around access, patient communications, messaging solutions and workload management at the same time.
Perhaps commissioners think we are looking for more work and often reply, ‘No thanks, we are just looking at online consultation and video consultation at the moment, messaging is done separately’. This is a missed opportunity for practices as they can’t make online consultation choices, without knowing what is happening to messaging, and buying telephony in isolation also results in overlap of features. Contracts have previously been procured from different budgets and end dates don’t align for renewals. And because some of the contracts are held with ICBs and others with Federations, PCNs or practices, we see an overlap in functionality and cost.
Tension then occurs when an ICB says, ‘But we bought this OC solution for you to save us money’ (i.e. SMS costs) and the Practices say ‘No, thanks, we prefer this other product, as it is easier for us to use and saves us time’. This sort of value often isn’t visible and it’s hard to quantify.
NHS Digital Commissioning And Procurement: Engagement Stage, Seeing The Other Perspective
Although some Commissioners engage well, others may have limited understanding, so they don’t feel or appreciate the direct benefits in terms of time saved in general practice. However, you can be sure, that the GP who has ‘too many clicks’ in a workflow knows this, especially when repeated hundreds of times a day or the Practice staff who need multiple logins to separate systems to monitor workloads.
The product supplier says, ‘We’ve made it easier for you to work in our system, not your clinical system’, then the commissioners say, ‘We can’t see your activity, so make it visible in your appointment book’, and so the double recording or lack of clarity on activity monitoring begins.
Don’t get me started on GPAD.
The holy grail is to find a new product that does most things, in fewer systems and everyone can see the workload, not just a slice of it.
We all meet some slick sales teams, with their product pitch and response ‘Of course our product system can do that’, but some features might just be in the next sprint, or worse, in roadmaps promised sometime in the next 12 months and yet not clearly understood, tested or ready to ship to market!
NHS Digital Commissioning And Procurement Rolling Over Contracts
Already, several commissioners have just re-contracted for a further 12 months or longer. That’s great if the product they have meets everyone’s needs and the supplier is still iterating and developing to keep pace with the interoperability and wider PCN and Neighbourhood team service requirements coming.
Where this isn’t great, either in user experience or value for money, is when the product teams have sat back, and not future-proofed designs because they have another 12-month breathing space. Or when the clunkiness of the internal user journey adds to the workload or requires the users to log in and out of multiple systems to complete their tasks.
What is also not great, is that new suppliers can’t get to the marketplace because they aren’t yet on the purchasing framework for Practices PCNs and Federations to buy from. So, practices and PCNs have two choices: stick with what they have and improve their internal process as best they can, then try to optimise use.
Or move and go ‘at risk’ financially and invest in a new product more suited to their needs, that can reduce some of the overlap, waste, and interoperability challenges, and we all know there isn’t a great deal of cash around in PCNs to do this.
NHS Digital Commissioning And Procurement: Where We Can Help
Last year we helped an ICB to reprocure their online and video consulting products by supporting the engagement with practice/PCNs and liaising with suppliers to showcase their products. When the Buying Catalogue is refreshed, it still can’t reflect the detailed features available in the newer products and that’s where Redmoor can help by setting up product ‘deep dives’ that add real value.
Practices can also ask all of the ‘how do you do A, B or C’ and then say, ‘Show Me’, which gets around the shiny salesman and also lets others see something that maybe they hadn’t thought about.
It gives us a chance to understand what the pain points are, so when we are asked to support implementation, we can optimise how the product will work, in line with a better experience for both the practice teams and the end user.
To help, we’ve packaged up our collective knowledge and experience and can support you if you wish to review your products. We can work closely with the NHS procurement hubs and support ICBs, Federations, and PCNs to do the engagement with practices, so you get the blend of commercial expertise on the contracting side and our operational knowledge and understanding of product capabilities.
Our procurement support service can walk you through three stages of moving to new Digital Solutions, to make sure you select the right products, engage with your practices and suppliers and maximise the adoption in your teams.
Drop us a line at hello@redmoorhealth.co.uk

Blog by Lisa Drake
Lisa supports commissioners at CCG/ICS & Regional level to help to deliver system change and modernise general practice. With almost 20 years experience in the NHS, as an ex-commissioner and Practice manager, Lisa’s work also involves advising practices and PCNs how to improve patients’ digital experience; how to deliver full range of GP Online services and streamline general practice workload. In addition to her role at Redmoor, Lisa remains in the NHS as a Digital Advisor in a practice in the Lake District.
Lisa is a mature student of the Open University specialising in Social Policy, Health and Care communications and relationships and is a member of the Expert Advisory Group for the Remote by Default Research with Nuffield Primary Care Health Sciences and University of Oxford.
Make an enquiry


